For Query & Appointment, Chandigarh +91-172-4637159 / 5018018, ![]() [email protected]
[email protected]
For Query & Appointment, Chandigarh +91-172-4637159 / 5018018, ![]() [email protected]
[email protected]
Jaundice refers to the yellow appearance of the skin that occurs with the deposition of bilirubin in the dermal and subcutaneous tissue. Normally in the body, bilirubin is processed through the liver, where it is conjugated to glucuronic acid by the enzyme uridine diphosphate glucuronyl transferase (UGT) 1A1. This conjugated form of bilirubin is then excreted into the bile and removed from the body via the gut. When this excretion process is low following birth, does not work efficiently, or is overwhelmed by the amount of endogenously produced bilirubin, the amount of bilirubin in the body increases, resulting in hyperbilirubinemia and jaundice.
Jaundice occurs in as many as 60% of all normal newborns within the first week of life. Jaundice in the newborn can occur from an underlying pathological condition, such as isoimmune hemolysis or an RBC enzyme deficiency. However, it is more commonly due to the normal physiological inability of the newborn infant to process bilirubin adequately due to the combined effects of increased RBC turnover and a transient deficit in bilirubin conjugation in the liver.This type of nonpathologic jaundice is referred to as physiologic jaundice of the newborn.
In most infants with physiologic jaundice, bilirubin concentrations do not rise to a point that requires treatment. However, in some infants with exaggerated physiologic jaundice, and in many infants with pathologic jaundice, bilirubin in the blood reaches very high concentrations that put the infant at risk for acute and chronic bilirubin encephalopathy (kernicterus). In these cases, treatment aimed at decreasing bilirubin concentration is required in order to avoid kernicterus. Etiologies of hyperbilirubinemia in newborns are provided in the image below.

Effective treatments to decrease bilirubin levels in infants with severe jaundice include phototherapy and exchange transfusion.
The effect of light on jaundice in neonates, and the ability of light to decrease serum bilirubin levels, was first described by Cremer et al in 1958. This observation led to the development of light sources for use in the treatment of infants with hyperbilirubinemia, a treatment now referred to as phototherapy. Since its inception, phototherapy has been effectively used as a relatively inexpensive and noninvasive method of treating neonatal hyperbilirubinemia. The decline in the number or exchange transfusions in recent years is, at least in part, likely a direct reflection of the effectiveness of phototherapy at treating hyperbilirubinemia. In modern neonatal ICUs (NICUs) exchange transfusions are rare and are only used as a rescue therapy to avoid kernicterus in newborns with severe jaundice when phototherapy is inadequate.
At its most basic, phototherapy refers to the use of light to convert bilirubin molecules in the body into water soluble isomers that can be excreted by the body. The absorption of light by normal bilirubin (4Z,15Z-bilirubin) results in the creation of 2 isomeric forms of bilirubin: structural isomers and configurational isomers. The main structural isomer of bilirubin is Z-lumirubin. The main configurational isomer of bilirubin is 4Z,15 E -bilirubin. Configurational isomerization is reversible, and structural isomerization is irreversible. Both the configurational and structural isomers of bilirubin are less lipophilic than normal bilirubin and can be excreted into bile without undergoing glucuronidation in the liver. Some of the configurational isomers of bilirubin, however, revert back to the native form after excretion into bile and can be reabsorbed via enterohepatic circulation in the gut. Structural bilirubin isomers, like Z-lumirubin, can also be excreted in the urine.
The absorptions of light by bilirubin also results in the generation of excited-state bilirubin molecules that react with oxygen to produce colorless oxidation products, or photooxidation products. This process occurs more slowly than configurational or structural isomerization. Photooxidation products are primarily excreted in the urine. The image below provides a schematic of the conversion of normal bilirubin to configurational isomers, structural isomers, and photooxidation products and the respective routes of excretion from the body.
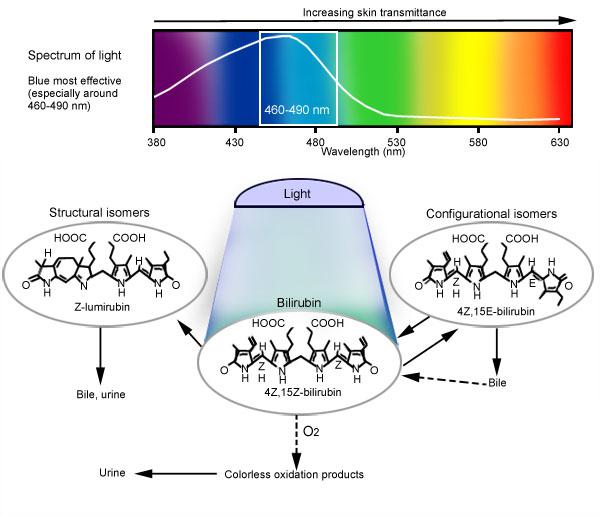
Mechanism of phototherapy: Blue-green light in the range of 460-490 nm is most effective for phototherapy. The absorption of light by the normal bilirubin (4Z,15Z-bilirubin) generates configuration isomers, structural isomers, and photooxidation products. The 2 principal photoisomers formed in humans are shown. Configurational isomerization is reversible and much faster than structural isomerization. Structural isomerization is slow and irreversible. Photooxidation occurs more slowly than both configurational and structural isomerization. Photooxidation products are excreted mainly in urine. Adapted from Maisel MJ, McDonagh AD. Phototherapy for Neonatal Jaundice.